3 min read
Dec 18, 2025
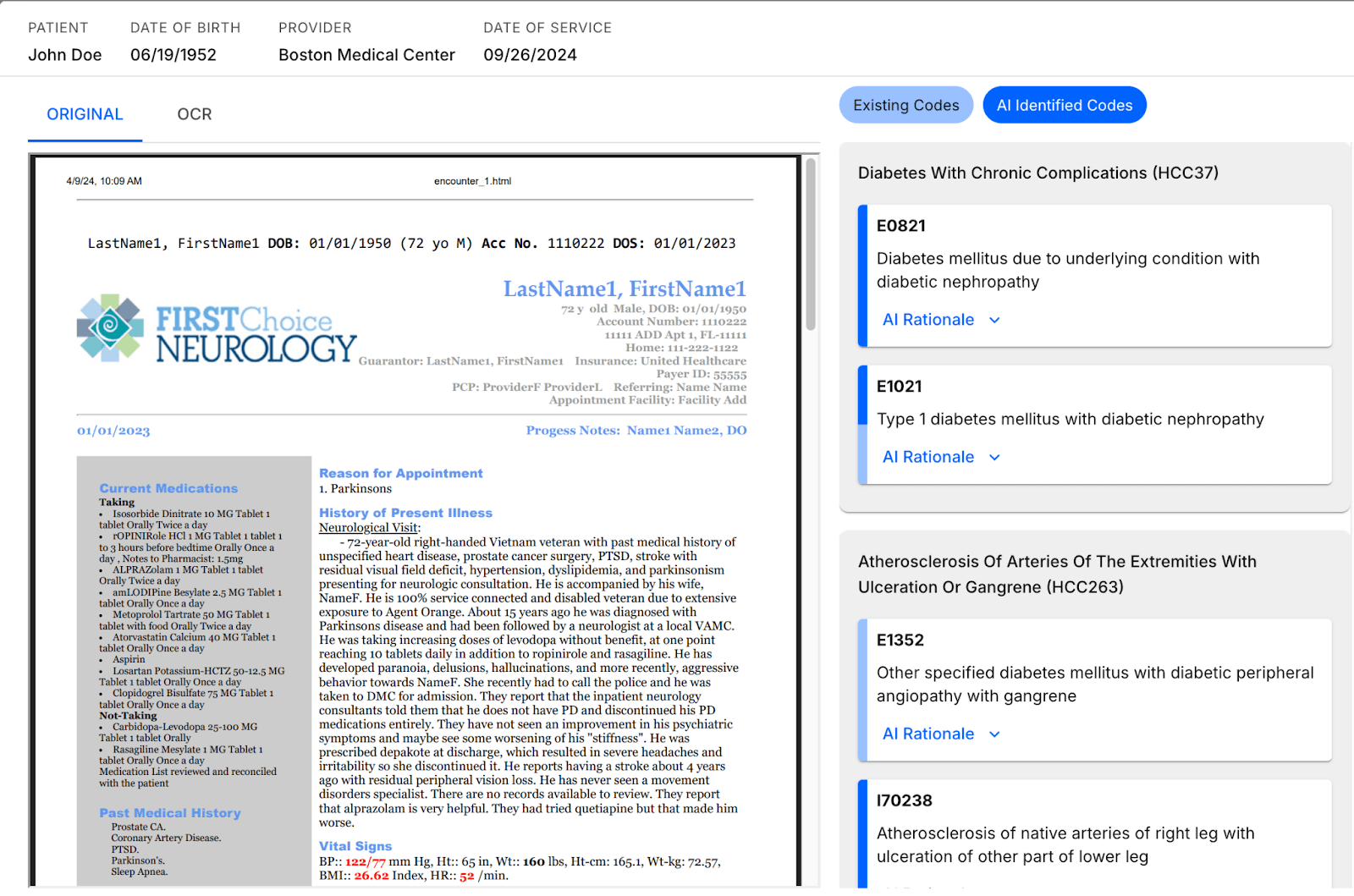
Can Your AI Tell Which Charts Actually Matter?
For years, risk adjustment was defined by a costly ultimatum: review 100% of charts or accept that revenue is being missed. Because there was no reliable technology to identify which charts have net new HCCs, organizations were forced to review the entire universe of charts to find maximum value. To mitigate the risk of human error, and because average coder recall hovers around ~80%, teams relied on expensive, multi-pass reviews.
A new model is now emerging, one that reframes AI not as a productivity tool layered onto existing workflows, but as a strategic mechanism for deciding where human effort creates value and, just as importantly, where it does not.
The End of the "Search Everything" Strategy
The traditional approach to risk adjustment relies on brute force: reviewing every chart to find every diagnosis. While previous generations of NLP tools attempted to assist this process by increasing code capture, they often lacked context, surfacing false positives that created more work rather than less.
The new model relies on a different premise: Most charts do not contain net-new HCCs.
By utilizing a generative AI platform trained to find all HCCs, and specifically net-new code capture, organizations can isolate the specific encounters that require human attention.
Complete Code Capture: The HealthMC system achieves ~99-100% recall for net-new HCC identification across all patient charts.
High Accuracy: Because the AI filters out the noise, the volume of charts requiring human review drops significantly.
Result: Organizations capture ~99-100% of accurate lift while reviewing only ~5% of charts.
The HealthMC Platform finds all HCCs in a chart and identifies the charts with novel HCCs for the patient, reducing coder review time by up to 95%.
Redefining the Human Workflow
Importantly, this model upgrades rather than replaces the coding team. Every net-new HCC identified by AI still requires human validation to confirm documentation and ensure audit readiness before submission to CMS.
The strategic shift lies in how coding teams are deployed. Instead of "searching a haystack," coders focus exclusively on validating high-likelihood opportunities.. This eliminates the need for redundant multi-pass cycles and allows coding experts to practice at the top of their license.
A New Economic Model for Healthcare Operations
When review volume drops by up to 95% and revenue capture remains intact, the financial implications are significant:
Higher marginal ROI per coder hour
Lower administrative overhead and operational costs
Fewer multi-pass review cycles
Faster cycle times and more predictable outputs
This model allows organizations to scale risk adjustment programs without linearly increasing headcount.
Beyond Retrospective Risk Adjustment
The impact of this new operating model extends well beyond retrospective coding. Any workflow where expert humans review clinical documentation can benefit from technology that prioritizes the charts that matter.
Applications include:
Concurrent Risk Adjustment: Identifying ambiguous cases for coder queries, future suspect diagnoses, and ensuring in-year documentation integrity.
Quality and HEDIS: Detecting gaps in care and confirming evidence of gap closure.
Clinical Operations: Supporting workflows in care management triage, population health, and utilization management.
In each case, the value lies not in automating judgment, but in directing it more intelligently.
The Path Forward
This moment represents a shift in how healthcare organizations deploy technology. The goal is no longer just to make teams faster, but to fundamentally reshape how work is allocated.
As we look toward the next phase of healthcare operations, the question for leadership is no longer whether AI can read charts, but whether your operating model is optimized to ignore the 95% of data that doesn't drive value.






